UMass Lowell public health professor studies aging, health inequities
Research shows connection between neighborhoods and health
Public Health Prof. Wenjun Li works with federal agencies and hospital systems to research the resources that contribute to healthy aging – and how access to those resources is affected by income, race and neighborhood conditions.
Li’s research group, the Health Statistics and Geography Lab, is also at the heart of a new biostatistics group at UMass Lowell that can offer statistical analysis to support other faculty, government agencies and private companies. As the group is growing, it is recruiting more professional staff, doctoral students and postdoctoral fellows.
Since joining the Zuckerberg College of Health Sciences last summer, Li has been collaborating with other faculty across campus on health issues throughout the lifespan. He looks forward to working closely with more faculty, student interns and community partners in the Merrimack Valley and southern New Hampshire, once the COVID-19 pandemic eases.
Li, who was previously based at UMass Medical School, teaches graduate courses in advanced biostatistics and quantitative research methods. He recently took the time to discuss his work.
Q: What is the focus of your aging research?
A: My passion always goes to public health and population health, using epidemiological, geographic and quantitative approaches. I work primarily with state and federal agencies to analyze data about community, social and neighborhood influences on health care, health behaviors and health outcomes, including prevention and treatment of chronic diseases, injuries and disabilities.
Q: What have you learned so far?
A: My most important finding is that the living environment plays a very important role in the likelihood of engaging in healthy behaviors, having chronic conditions and being injured or disabled. A better neighborhood environment supports healthy living and improves older people’s health and general well-being.
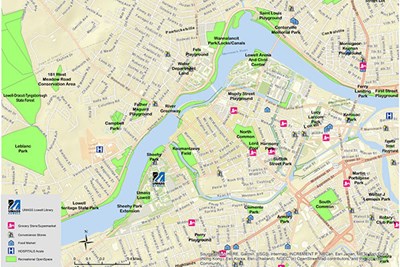
The living environment has two components: social and physical. Social factors include crime and safety, civic involvement, social isolation or connection, economic and racial disparities and access to health care and mental health resources, including preventive and rehabilitation care. The physical environment includes things like access to grocery stores with healthy food, access to a center or council on aging and resources for physical exercise, such as parks and sidewalks or gyms.
Access to those resources and services has a profound impact on people’s ability to age without being displaced and prematurely admitted to a nursing home. Most people want to stay in their own home – the question is how to help them do that.
Q: Both the social and physical living environments implicate race and socioeconomic status. How does your research address that?
A: Socioeconomic disparities in access to services is tremendous, so we work with public health agencies to figure out the most effective ways for them to address those gaps.
Typically, we analyze access to health resources by socioeconomic status, level of education, race and geographic location. Right now, we are working on the Healthy Aging and Neighborhood Study under a five-year, nearly $4 million grant from the National Institute on Aging. We’re comparing health and access to critical living resources and services in urban, suburban and rural areas in central Massachusetts, and we’re analyzing geographic disparities right down to the neighborhood level.
Q: What other major projects are you working on now?
A: We are assisting the Centers for Disease Control and Prevention and the National Association of Chronic Disease Directors in developing a prototype for a national system to determine the prevalence of chronic diseases and conditions such as diabetes, high blood pressure and heart disease in different locations and populations. We’re partnering with four hospital systems across the country to extract de-identified bulk data directly from their electronic medical records – and then analyzing it. Our share of this chronic disease surveillance system grant is $1.2 million.
Public Health Chair Dan Berlowitz and I are also co-investigators on a grant led by Computer Science Prof. Hong Yu that aims to help the Veterans Health Administration identify veterans who are at high risk of suicide. We will develop predictive models by looking at behavior issues, access to and use of treatments, and social factors such as whether or not someone is employed or has a disability. We hope that will help the VA offer more targeted prevention and intervention services.
Q: How are students involved in your research?
A: In Worcester, our lab has had a long tradition of hosting internship programs for high school students, undergraduates, graduate students and post-doctoral fellows. Over the past 15 years, we’ve hosted about 70 student interns, with all of their positions funded by federal grants.
Once the campus is fully open, we’re planning to restart our intern program here. We plan to engage local high schools and help the university expand its recruitment – and to get more students who are socioeconomically and racially diverse.
It’s our way of trying to attract these students to health sciences research. Many of our interns have gone on to top medical and graduate schools. Several of my former interns now work in my lab, too. They came, they loved it and they decided to stay as my professional staff.